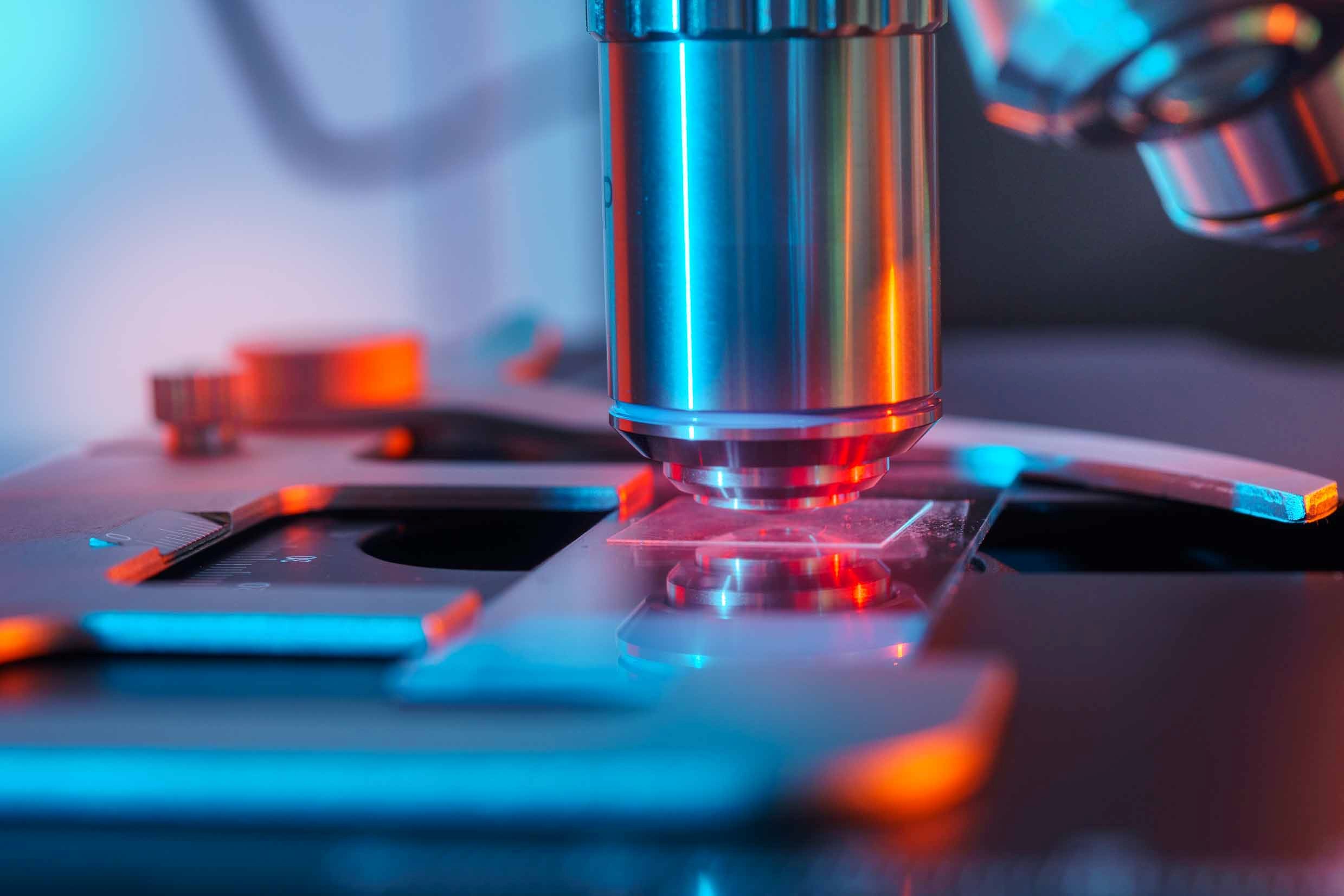
Microscope technology has evolved tremendously over the past several decades, far beyond simply adjusting light intensity, changing objectives, and positioning and focusing a specimen — with digital telepathology, anyone with an internet connection can review microscopic samples remotely. Let’s examine what real-time telepathology is and the advantages that microscopes like the ACCU-SCOPE RC500 have over traditional models.
What Is Digital Pathology?
Digital pathology first emerged in the 1980s and has advanced considerably since its introduction. Thanks to numerous technological advancements over the years, it is now an indispensable part of countless institutions.
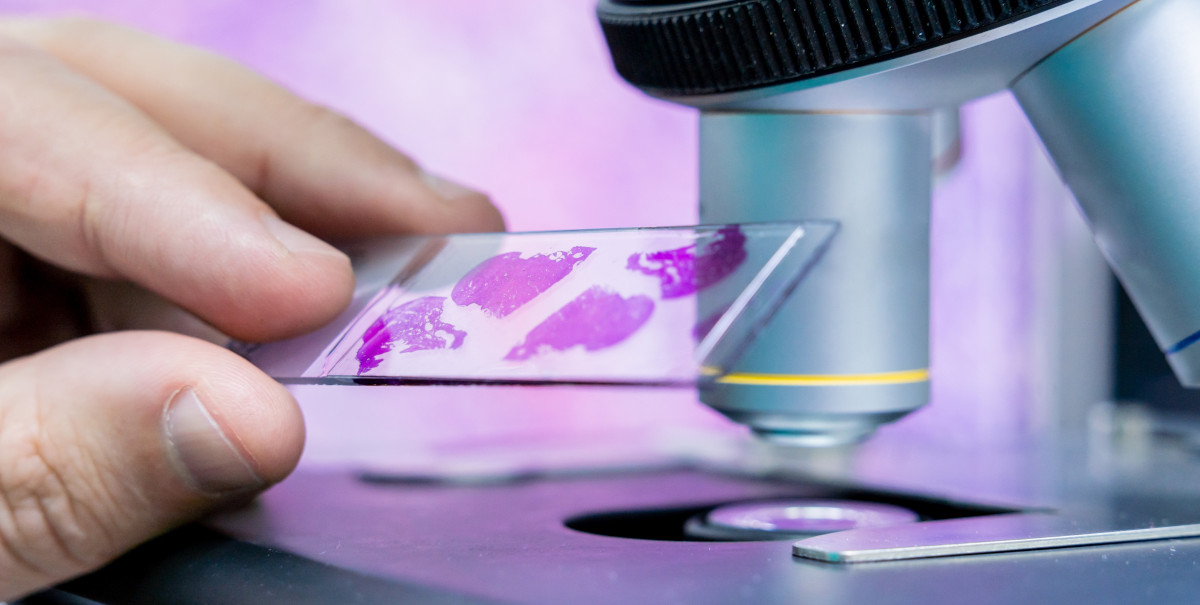
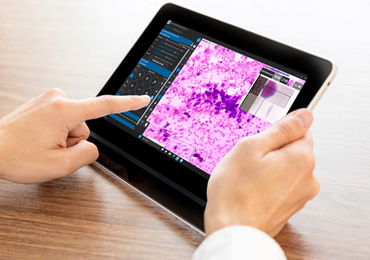
In its infancy, digital pathology relied on the capture and sharing of static images with the remote reviewer. Digital pathology has evolved to utilize whole-slide imaging to scan and digitize entire glass slides, then store and share the digital slide files via the internet. In addition to capturing static specimen images, some digital pathology technology can capture and permit the viewing (streaming) of live images as well.
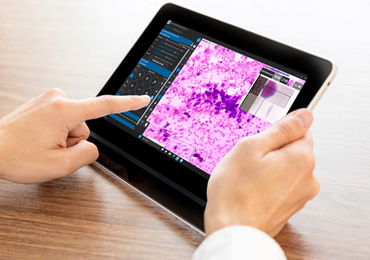
The creation of high-quality specimen imagery allows individuals to easily view, analyze, and manage pathology samples on an electronic device of their choice. In short, digital telepathology allows for remote functionality over long distances so long as there is an established internet connection.
The Benefits of Real-Time Telepathology
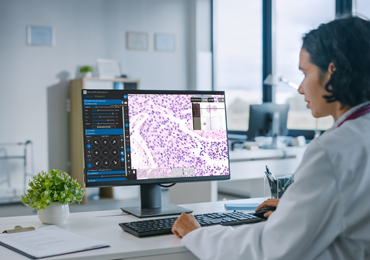
One of the greatest strengths of real-time telepathology is that it allows a remote user to access and review live images of patient slides from long (or not-so-long) distances. This is particularly useful given the increasingly constrained availability of pathologists, including when they are not local to the hospital labs for in-person viewing.
For example, real-time telepathology enables healthcare professionals to review slides from patient cases in rural regions without having to transfer the physical slides to a faraway hospital. Given how delays in diagnosis can be dangerous, real-time telepathology has the potential to save lives through its accessibility to pathologists, regardless of their location. Remote functionality also allows remote viewers to review samples from biopsies and fine needle aspirates (FNA) while the patient is still in the operating room.
In addition, this innovative approach to pathology can help reduce costs and improve the speed and quality of patient care. It allows sub-specialists to review difficult cases or provide second opinions and enhances the coordination and communication between all medical personnel in a particular patient’s care team. The accelerated decision-making brought about by this remote collaboration leads to greater productivity, improving patient care as a result.
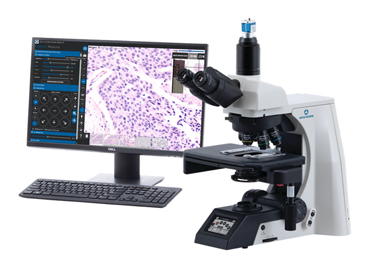
The ACCU-SCOPE RC500 is a remote collaboration system designed for real-time telepathology and consists of a motorized microscope, motorized stage, computer, and software. By logging into the RC500 computer desktop, a remote viewer has full control of the microscope and specimen position – the only operation the remote reviewer cannot do is place the slide on the stage. It’s worth noting that the RC500 can also function as a traditional microscope when not being used for telepathology, allowing for greater flexibility and multipurpose usage in the laboratory.
What Is Rapid On-Site Evaluation?
Rapid On-Site Evaluation (ROSE) refers to the near-immediate review of a patient sample by a pathologist. Tissue biopsies are taken from a patient in the operating room (OR), the biopsies are prepared and reviewed by a pathologist, all while the patient is still in the OR. Normally, this would involve the pathologist visiting the pathology (frozen section) laboratory located near the OR. Thanks to real-time telepathology, the pathologist doesn’t need to come down to the frozen section lab to review the sample — rather, they can do so quickly and conveniently from their office.
OSEA (On-Site Evaluation of Adequacy) is one version of ROSE in which fine needle aspiration (FNA) types of biopsies are reviewed to provide a quick determination of whether there is sufficient (adequate) cellular content for a cytopathologist or pathologist to render a diagnosis, classification or disease stage of the specimen. As pathologists are not always readily available to review a ROSE case, a cytopathologist or cytotechnologist may also not be available to review OSEA cases and, therefore, remote telepathology can play a critical part in providing fast access to the medical experts to determine sample adequacy.
Applications of Remote Telepathology
There are numerous medical disciplines that utilize remote telepathology, including pathology, cytopathology, hematopathology, anatomic pathology, microbiology, dermatopathology, and many more. As such, the seamless automation and remote viewership of this technology naturally lead to a diverse range of applications.
For example, remote telepathology can be utilized in healthcare settings for patient diagnosis, clinical research, and even resident training. In addition, this technology is a highly effective tool in educational environments beyond just healthcare. Digital images can be acquired from any specimen, saved to a network or the cloud, and then accessed from any device, allowing students to easily view the digitized samples outside of class. Furthermore, the digitized samples ensure that all students experience the same “slides” and the same locations/features on the slides, thereby standardizing the learning experience.
If You’re Interested in Learning More About an RC500 Microscope for Your Institution, Contact ACCU-SCOPE Today
To bring the benefits of remote functionality to your laboratory, reach out to ACCU-SCOPE. In addition to the RC500 microscope, we also supply traditional microscopes, high-quality digital imaging cameras, and more. Contact us today for further information and to place an order for your organization.